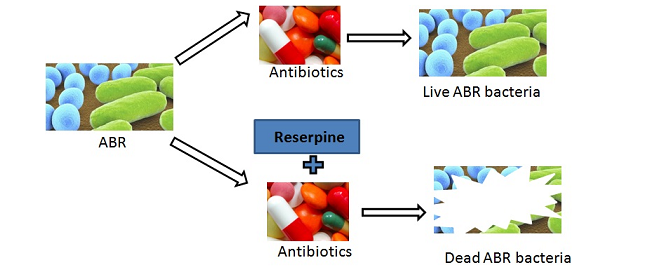
Inhibitory effects of reserpine against efflux pump activity of antibiotic resistance bacteria
Abstract
Keywords
References
T. Christian, R.J. Schneider, H.A. Färber, D. Skutlarek, M.T. Meyer, H.E. Goldbach. Determination of Antibiotic Residues in Manure, Soil, and Surface Waters. Acta hydrochim hydrobiol, 2003, 31, 36-44.
C. Walsh, Antibiotics: Actions, Origins, Resistance. ASM Press, 2003.
A. Tamrakar, A. Singh, M. Chodhrary, P. Kodgire. Fighting with Gram-negative enemy: Can outer membrane proteins aid in the rescue? Chem. Biol. Lett., 2017, 4(1), 9-19.
S. Mullin, N. Mani, T.H. Grossman. Inhibition of Antibiotic Efflux in Bacteria by the Novel Multidrug Resistance Inhibitors Biricodar (VX-710) and Timcodar (VX-853). Antimicrob Agents Chemother, 2004, 48, 4171-4176.
O. Lomovskaya, M.S. Warren, A. Lee, J. Galazzo, R. Fronko, M. Lee, J. Blais. Identification and characterization of inhibitors of multidrug resistance efflux pumps in Pseudomonas aeruginosa: novel agents for combination therapy. Antimicrob Agents Chemother, 2001, 45, 105-116.
P.N. Markham, E. Westhaus, K. Klyachko, M.E. Johnson, A.A. Neyfakh. Multiple Novel Inhibitors of the NorA Multidrug Transporter of Staphylococcus aureus. Antimicrob Agents Chemother, 1999, 43, 2404-2408.
A.A. Neyfakh, C.M. Borsch, G.W. Kaatz. Fluoroquinolone resistance protein NorA of Staphylococcus aureus is a multidrug efflux transporter. Antimicrob Agents Chemother, 1993, 37, 128-129.
W, J. Lee, M.N. Chen, T. K.Huda, T. Uroda, T. Mizushima, T. Tsuchiya. Functional cloning and expression of emeA, and characterization of EmeA, a multidrug efflux pump from Enterococcus faecalis. Biol Pharm Bull, 2003, 26, 266–270
M.J. Gill, N.P. Brenwald, R. Wise. Identification of an efflux pump gene, pmrA, associated with fluoroquinolone resistance in Streptococcus pneumoniae. Antimicrob Agents Chemother, 1999, 43, 187-189.
A.A. Neyfakh,V.E. Bidnenko, L.B. Chen. Efflux-mediated multidrug resistance in Bacillus subtilis: similarities and dissimilarities with the mammalian system. Proc Natl Acad Sci USA, 1991, 88, 4781–4785.
T.S. Dhanarani, C. Shankar, J. Park, M. Dexilin, R.R. Kumar, Thamaraiselvi K. Study on acquisition of bacterial antibiotic resistance determinants in poultry litter. Poult Sci, 2009, 88, 1381-1387.
M. Teresa Tejedor, J.L. MartÃn, M. Navia, J. Freixes, J. Vila. Mechanisms of fluoroquinolone resistance in Pseudomonas aeruginosa isolates from canine infections. Vet Microbiol, 2003, 94, 295-301.
G.W. Kaatz, S.M. Seo, C.A. Ruble. Efflux-mediated fluoroquinolone resistance in Staphylococcus aureus. Antimicrob Agents Chemother, 1993, 37, 1086-1094.
G.W. Kaatz, S.M. Seo. Inducible NorA-mediated multidrug resistance in Staphylococcus aureus. Antimicrob Agents Chemother, 1995,39,2650-2655.
A. Thorarensen, A.L. Presley-Bodnar, K.R. Marotti, T.P. Boyle, C.L. Heckaman, M.J. Bohanon, P.K. Tomich, G.E. Zurenko, M.T. Sweeney, B.H. Yagi. 3-Arylpiperidines as potentiators of existing antibacterial agents. Bioorg Med Chem Lett, 2001, 11, 1903-1906.
B.A. Mitchell, I.T. Paulsen, M.H. Brown, R.A. Skurray. Bioenergetics of the staphylococcal multidrug export protein QacA. Identification of distinct binding sites for monovalent and divalent cations. J Biol Chem, 1999, 274, 3541-3548.
M. Putman, L.A. Koole, H.W Veen, W.N. Konings. The secondary multidrug transporter LmrP contains multiple drug interaction sites. Biochemistry, 1999, 38, 13900-13905.
A. Aygül. The importance of efflux systems in antibiotic resistance and efflux pump inhibitors in the management of resistance]. Mikrobiyoloji bulteni, 2015, 49(2), 278-291.
M.A.S. Moreira, E.C. Souza, C.A Moraes. Multidrug efflux systems in Gram-negative bacteria. Brazilian Journal of Microbiology, 2004, 35, 19-28.
F.J. Schmitz, A.C. Fluit, M. Lückefahr, B. Engler, B. Hofmann, J. Verhoef, H.P. Heinz, U. Hadding, ME. Jones. The effect of reserpine, an inhibitor of multidrug efflux pumps, on the in-vitro activities of ciprofloxacin, sparfloxacin and moxifloxacin against clinical isolates of Staphylococcus aureus. J Antimicrob Chemother, 1998, 42, 807-810.
A. Beceiro, M. Tomás, G. Bou, G. Antimicrobial resistance and virulence: a successful or deleterious association in the bacterial world?. Clinical microbiology reviews, 2013, 26(2), 185-230.
K. Goud, N. Veldurthi, M. Vithal, G. Reddy. Characterization and evaluation of biological and photocatalytic activities of selenium nanoparticles synthesized using yeast fermented broth. Applied Nanomedicine, 2016, 1(1), 12-19.
H. Jafri, F. Husain, I. Ahmad. Antibacterial and antibiofilm activity of some essential oils and compounds against clinical strains of Staphylococcus aureus. J. Biomed. Therapeutic Sci., 2014, 1(1), 65-71.
ISSN 2347–9825
Authors/visitors are advised to use Firefox browser for better experience of journal site.
Open Access: Researcher from developing/low economy countries can access the jorunal contents through WHO-HINARI .
 ISSN 2347-9825
ISSN 2347-9825

