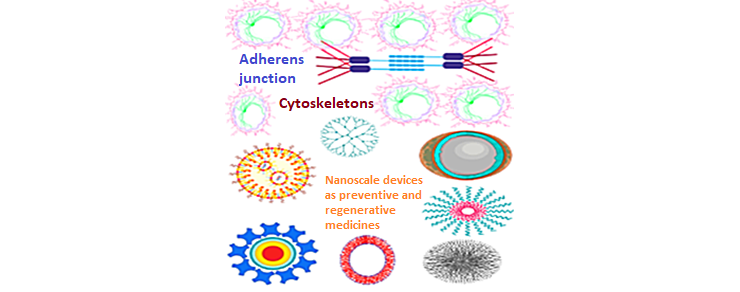
Nanobiomaterials, nanobiomechanics and tissue bioengineering for advanced regenerative therapeutics: present and future perspectives
Abstract
Keywords
References
J.L. Olson, A. Atala, J.J. Yoo. Tissue Engineering: Current Strategies and Future Directions. Chonnam Med. J. 2011, 47 (1), 1.
P.X. Ma. Biomimetic materials for tissue engineering. Adv. Drug Deliv. Rev. 2008, 60 (2), 184–198.
A.J. Salgado, J.M. Oliveira, A. Martins, et al. Tissue Engineering and Regenerative Medicine. In International Review of Neurobiology; 2013; Vol. 108, pp 1–33.
S.K. Misra, P. Moitra, B.S. Chhikara, P. Kondaiah, S. Bhattacharya. Loading of single-walled carbon nanotubes in cationic cholesterol suspensions significantly improves gene transfection efficiency in serum. J. Mater. Chem. 2012, 22 (16), 7985–7998.
B.S. Chhikara, S.K. Misra, S. Bhattacharya. CNT loading into cationic cholesterol suspensions show improved DNA binding and serum stability and ability to internalize into cancer cells. Nanotechnology 2012, 23 (6), 065101.
S. Guven, P. Chen, F. Inci, et al. Multiscale assembly for tissue engineering and regenerative medicine. Trends Biotechnol. 2015, 33 (5), 269–279.
A. Atala. Tissue engineering of reproductive tissues and organs. Fertil. Steril. 2012, 98 (1), 21–29.
M.W. Tibbitt, K.S. Anseth. Hydrogels as extracellular matrix mimics for 3D cell culture. Biotechnol. Bioeng. 2009, 103 (4), 655–663.
G. Vunjak-Novakovic, K.O. Lui, N. Tandon, K.R. Chien. Bioengineering Heart Muscle: A Paradigm for Regenerative Medicine. Annu. Rev. Biomed. Eng. 2011, 13 (1), 245–267.
G.C. Gurtner, M.J. Callaghan, M.T. Longaker. Progress and Potential for Regenerative Medicine. Annu. Rev. Med. 2007, 58 (1), 299–312.
S.J. Forbes, N. Rosenthal. Preparing the ground for tissue regeneration: from mechanism to therapy. Nat. Med. 2014, 20 (8), 857–869.
J.D. Boerckel, D.E. Mason, A.M. McDermott, E. Alsberg. Microcomputed tomography: approaches and applications in bioengineering. Stem Cell Res. Ther. 2014, 5 (6), 144.
S.W. Lane, D.A. Williams, F.M. Watt. Modulating the stem cell niche for tissue regeneration. Nat. Biotechnol. 2014, 32 (8), 795–803.
G. Albrecht. Molecular, Cellular, and Tissue Engineering. In Encyclopedia of Disability; 2014.
J. Chen. Nanobiomechanics of living cells: a review. Interface Focus 2014, 4 (2), 20130055.
K.-K. Liu, M.L. Oyen. Nanobiomechanics of living materials. Interface Focus 2014, 4 (2), 20140001.
A. Ikai. Nanobiomechanics of proteins and biomembrane. Philosophical Transactions of the Royal Society B: Biological Sciences. 2008, pp 2163–2171.
A. Mata. Micro and nanotechnologies for bioengineering regenerative medicine scaffolds. Int. J. Biomed. Eng. Technol. 2011, 5 (2–3), 266–291.
Y. Zhao, N.T. Feric, N. Thavandiran, S.S. Nunes, M. Radisic. The Role of Tissue Engineering and Biomaterials in Cardiac Regenerative Medicine. Canadian Journal of Cardiology. 2014, pp 1307–1322.
N.H. Romano, D. Sengupta, C. Chung, S.C. Heilshorn. Protein-engineered biomaterials: Nanoscale mimics of the extracellular matrix. Biochimica et Biophysica Acta - General Subjects. 2011, pp 339–349.
H. Bae, H. Chu, F. Edalat, et al. Development of functional biomaterials with micro- and nanoscale technologies for tissue engineering and drug delivery applications. Journal of Tissue Engineering and Regenerative Medicine. 2014, pp 1–14.
S.A. Guelcher. Biodegradable polyurethanes: Synthesis and applications in regenerative medicine. Tissue Engineering - Part B: Reviews. 2008, pp 3–17.
A. Albanese, C.D. Walkey, J.B. Olsen, et al. Secreted biomolecules alter the biological identity and cellular interactions of nanoparticles. ACS Nano 2014, 8 (6), 5515–5526.
A.R. Amini, C.T. Laurencin, S.P. Nukavarapu. Bone tissue engineering: Recent advances and challenges. Crit. Rev. Biomed. Eng. 2012, 40 (5), 363–408.
M. Rolandi, R. Rolandi. Self-assembled chitin nanofibers and applications. Advances in Colloid and Interface Science. 2014, pp 216–222.
T.A. Einhorn. Bone Regeneration and Repair. J. Bone Jt. Surg. 2006, 88 (2), 469–470.
L. Andolfi, M. Lazzarino, V. Masciotti, Y. Qi, J. Hu. Nanobiomechanics and Mechanotransduction of Sensory Neurons. Biophys. J. 2015, 108 (2), 560a.
M. Sebastian Mannoor. Bionic Nanosystems. Diss. Abstr. Int. 2014, 75 (10), 195.
A. Bergmann, H. Steller. Apoptosis, Stem Cells, and Tissue Regeneration. Sci. Signal. 2010, 3 (145), re8–re8.
M. Reimann, E. Bonifacio, M. Solimena, et al. An update on preventive and regenerative therapies in diabetes mellitus. Pharmacology and Therapeutics. 2009, pp 317–331.
S.Q. Liu. Bioregenerative Engineering: Principles and Applications; 2006.
B. Yanez-Soto, S.J. Liliensiek, J.Z. Gasiorowski, C.J. Murphy, P.F. Nealey. The influence of substrate topography on the migration of corneal epithelial wound borders. Biomaterials 2013, 34 (37), 9244–9251.
J. Venugopal, P. Vadgama, T.S.S. Kumar, S. Ramakrishna. Biocomposite nanofibres and osteoblasts for bone tissue engineering. Nanotechnology 2007, 18 (5), 055101.
L. Petrovic, A.K. Schlegel, S. Schultze-Mosgau, J. Wiltfang. Different substitute biomaterials as potential scaffolds in tissue engineering. Int. J. Oral Maxillofac. Implant. 2006, 21 (2), 225–231.
F. Guilak, D.M. Cohen, B.T. Estes, et al. Control of Stem Cell Fate by Physical Interactions with the Extracellular Matrix. Cell Stem Cell. 2009, pp 17–26.
D.E. Ingber, V.C. Mow, D. Butler, et al. Tissue engineering and developmental biology: Going biomimetic. In Tissue Engineering; 2006; Vol. 12, pp 3265–3283.
L.B. Thomsen, A. Burkhart, T. Moos. A Triple Culture Model of the Blood-Brain Barrier Using Porcine Brain Endothelial cells, Astrocytes and Pericytes. PLoS One 2015, 10 (8), e0134765.
C.M. Valmikinathan, J. Tian, J. Wang, X. Yu. Novel nanofibrous spiral scaffolds for neural tissue engineering. J. Neural Eng. 2008, 5 (4), 422–432.
F. Rosso, A. Giordano, M. Barbarisi, A. Barbarisi. From Cell-ECM Interactions to Tissue Engineering. J. Cell. Physiol. 2004, 199 (2), 174–180.
M. Manzano, M. Vallet-RegÃ. Revisiting bioceramics: Bone regenerative and local drug delivery systems. Progress in Solid State Chemistry. 2012, pp 17–30.
C.J. Wilson, R.E. Clegg, D.I. Leavesley, M.J. Pearcy. Mediation of biomaterial-cell interactions by adsorbed proteins: A review. Tissue Engineering. 2005, pp 1–18.
R.P. Pirraco, A.P. Marques, R.L. Reis. Cell interactions in bone tissue engineering. Journal of Cellular and Molecular Medicine. 2010, pp 93–102.
Z. Sheikh, S. Najeeb, Z. Khurshid, et al. Biodegradable materials for bone repair and tissue engineering applications. Materials. 2015, pp 5744–5794.
H.S. Hung, H.C. Chen, C.H. Tsai, S.Z. Lin. Novel approach by nanobiomaterials in vascular tissue engineering. Cell Transplantation. 2011, pp 63–70.
M. Mastri, Z. Shah, T. McLaughlin, et al. Activation of Toll-like receptor 3 amplifies mesenchymal stem cell trophic factors and enhances therapeutic potency. Am. J. Physiol. Cell Physiol. 2012, 303 (10), C1021-33.
M. Mastri. Cellular and molecular mechanisms in myocardial regeneration, 2013.
G.S. Schultz, G.A. Chin, L. Moldawer, R.F. Diegelmann. Principles of wound healing. In Mechanisms of Vascular Disease: A Reference Book for Vascular Specialists; 2011; pp 423–450.
E.S. White, A.R. Mantovani. Inflammation, wound repair, and fibrosis: Reassessing the spectrum of tissue injury and resolution. Journal of Pathology. 2013, pp 141–144.
A. Camelo, R. Dunmore, M.A. Sleeman, D.L. Clarke. The epithelium in idiopathic pulmonary fibrosis: breaking the barrier. Front. Pharmacol. 2014, 4, 0173.
J. Mann, D.A. Mann. Epigenetic regulation of wound healing and fibrosis. Curr. Opin. Rheumatol. 2013, 25 (1), 101–107.
G.C. Gurtner, S. Werner, Y. Barrandon, M.T. Longaker. Wound repair and regeneration. Nature. 2008, pp 314–321.
R. Dimitriou, E. Jones, D. McGonagle, P. V. Giannoudis. Bone regeneration: current concepts and future directions. BMC Med. 2011, 9 (1), 66.
P. Martin. Wound healing - Aiming for perfect skin regeneration. Science (80-. ). 1997, 276 (5309), 75–81.
J.D. Humphrey, E.R. Dufresne, M.A. Schwartz. Mechanotransduction and extracellular matrix homeostasis. Nat. Rev. Mol. Cell Biol. 2014, 15 (12), 802–812.
G.S. Schultz, A. Wysocki. Interactions between extracellular matrix and growth factors in wound healing. Wound Repair and Regeneration. 2009, pp 153–162.
H.K. Kleinman, D. Philp, M.P. Hoffman. Role of the extracellular matrix in morphogenesis. Curr. Opin. Biotechnol. 2003, 14 (5), 526–532.
C. Colnot. Cellular and molecular interactions regulating skeletogenesis. Journal of Cellular Biochemistry. 2005, pp 688–697.
C. Fania, L. Anastasia, M. Vasso, et al. Proteomic signature of reversine-treated murine fibroblasts by 2-D difference gel electrophoresis and MS: Possible associations with cell signalling networks. Electrophoresis 2009, 30 (12), 2193–2206.
L. Ricotti, T. Fujie, V. Pensabene, A. Menciassi. Bioengineering applications of ultra-thin poly(lactic acid) nanofilms towards cellbased smart biomaterials. In Polylactic Acid: Synthesis, Properties and Applications; 2012; pp 309–323.
A.R. Shrivats, M.C. McDermott, J.O. Hollinger. Bone tissue engineering: State of the union. Drug Discovery Today. 2014, pp 781–786.
M. Ramalingam, E. Jabbari, S. Ramakrishna, A. Khademhosseini. Micro and Nanotechnologies in Engineering Stem Cells and Tissues; John Wiley and Sons, 2013.
T. Osathanon, P. Pavasant, C. Giachelli. Notch signaling biomaterials and tissue regeneration; 2014.
L.A. Dobrzański. Applications of newly developed nanostructural and microporous materials in biomedical, tissue and mechanical engineering. Arch. Mater. Sci. Eng. 2015, 76 (2), 53–114.
B. Rolfe, J. Mooney, B. Zhang, et al. The Fibrotic Response to Implanted Biomaterials: Implications for Tissue Engineering. In Regenerative Medicine and Tissue Engineering - Cells and Biomaterials; InTech, 2011.
D. Singh, D. Singh, S. Zo, S.S. Han. Nano-biomimetics for nano/micro tissue regeneration. J. Biomed. Nanotechnol. 2014, 10 (10), 3141–3161.
B.S. Chhikara, D. Mandal, K. Parang. Synthesis, anticancer activities, and cellular uptake studies of lipophilic derivatives of doxorubicin succinate. J. Med. Chem. 2012, 55 (4), 1500–1510.
B.S. Chhikara, K. Parang. Development of cytarabine prodrugs and delivery systems for leukemia treatment. Expert Opin. Drug Deliv. 2010, 7 (12), 1399–1414.
B.S. Chhikara, N. St. Jean, D. Mandal, A. Kumar, K. Parang. Fatty acyl amide derivatives of doxorubicin: Synthesis and in vitro anticancer activities. Eur. J. Med. Chem. 2011, 46 (6), 2037–2042.
A. Nasrolahi Shirazi, R. Tiwari, B.S. Chhikara, D. Mandal, K. Parang. Design and biological evaluation of cell-penetrating peptide-doxorubicin conjugates as prodrugs. Mol. Pharm. 2013, 10 (2), 488–499.
B.S. Chhikara, D. Mandal, K. Parang. Synthesis and evaluation of fatty acyl ester derivatives of cytarabine as anti-leukemia agents. Eur. J. Med. Chem. 2010, 45 (10), 4601–4608.
F. Croisier, C. Jérôme. Chitosan-based biomaterials for tissue engineering. European Polymer Journal. 2013, pp 780–792.
Y.J. Seol, H.W. Kang, S.J. Lee, A. Atala, J.J. Yoo. Bioprinting technology and its applications. European Journal of Cardio-thoracic Surgery. 2014, pp 342–348.
C.L. Randall, T.G. Leong, N. Bassik, D.H. Gracias. 3D lithographically fabricated nanoliter containers for drug delivery. Advanced Drug Delivery Reviews. 2007, pp 1547–1561.
C.D. Reyes, T.A. Petrie, K.L. Burns, Z. Schwartz, A.J. GarcÃa. Biomolecular surface coating to enhance orthopaedic tissue healing and integration. Biomaterials 2007, 28 (21), 3228–3235.
L. Zhang, T.J. Webster. Nanotechnology and nanomaterials: Promises for improved tissue regeneration. Nano Today. 2009, pp 66–80.
C. Shi, Y. Zhu, X. Ran, et al. Therapeutic Potential of Chitosan and Its Derivatives in Regenerative Medicine1 1 This work was supported by “973†programs on severe trauma (NO. 1999054205 and NO. 2005CB522605) from the Ministry of Science and Technology of China. J. Surg. Res. 2006, 133 (2), 185–192.
K. Bott, Z. Upton, K. Schrobback, et al. The effect of matrix characteristics on fibroblast proliferation in 3D gels. Biomaterials 2010, 31 (32), 8454–8464.
M. Kerschensteiner, M.E. Schwab, J.W. Lichtman, T. Misgeld. In vivo imaging of axonal degeneration and regeneration in the injured spinal cord. Nat. Med. 2005, 11 (5), 572–577.
H.K. Agarwal, B.S. Chhikara, S. Bhavaraju, et al. Emtricitabine prodrugs with improved anti-hiv activity and cellular uptake. Mol. Pharm. 2013, 10 (2), 467–476.
V.K. Rao, R. Tiwari, B.S. Chhikara, et al. Copper triflate-mediated synthesis of 1,3,5-triarylpyrazoles in [bmim][PF6] ionic liquid and evaluation of their anticancer activities. RSC Adv. 2013, 3 (35), 15396–15403.
H.K. Agarwal, B.S. Chhikara, M.J. Hanley, et al. Synthesis and biological evaluation of fatty acyl ester derivatives of (-)-2′,3′-dideoxy-3′-thiacytidine. J Med Chem 2012, 55 (10), 4861–4871.
H.K. Agarwal, B.S. Chhikara, M. Quiterio, G.F. Doncel, K. Parang. Synthesis and anti-HIV activities of glutamate and peptide conjugates of nucleoside reverse transcriptase inhibitors. J Med Chem 2012, 55 (6), 2672–2687.
A.M. Alkilany, S.E. Lohse, C.J. Murphy. The gold standard: Gold nanoparticle libraries to understand the nano-bio interface. Acc. Chem. Res. 2013, 46 (3), 650–661.
B. Pelaz, G. Charron, C. Pfeiffer, et al. Interfacing engineered nanoparticles with biological systems: Anticipating adverse nano-bio interactions. Small. 2013, pp 1573–1584.
A.E. Nel, L. Mädler, D. Velegol, et al. Understanding biophysicochemical interactions at the nano-bio interface. Nature Materials. 2009, pp 543–557.
L. Shang, K. Nienhaus, G.U. Nienhaus. Engineered nanoparticles interacting with cells: Size matters. Journal of Nanobiotechnology. 2014.
S. Sowmya, J.D. Bumgardener, K.P. Chennazhi, S. V. Nair, R. Jayakumar. Role of nanostructured biopolymers and bioceramics in enamel, dentin and periodontal tissue regeneration. Progress in Polymer Science. 2013, pp 1748–1772.
C. Wilson, A. Magnaudeix, T. Naves, et al. The Ins and Outs of Nanoparticle Technology in Neurodegenerative Diseases and Cancer. Curr. Drug Metab. 2015, 16 (8), 609–632.
Y. Shi, Z. Xue, X. Wang, L. Wang, A. Wang. Removal of methylene blue from aqueous solution by sorption on lignocellulose-g-poly(acrylic acid)/montmorillonite three-dimensional cross-linked polymeric network hydrogels. Polym. Bull. 2013, 70 (4), 1163–1179.
A. Béduer, C. Vieu, F. Arnauduc, et al. Engineering of adult human neural stem cells differentiation through surface micropatterning. Biomaterials 2012, 33 (2), 504–514.
G.A.A. Saracino, D. Cigognini, D. Silva, A. Caprini, F. Gelain. Nanomaterials design and tests for neural tissue engineering. Chem. Soc. Rev. 2013, 42 (1), 225–262.
C.S. Yun, G.A. Khitrov, D.E. Vergona, N.O. Reich, G.F. Strouse. Enzymatic manipulation of DNA-nanomaterial constructs. J. Am. Chem. Soc. 2002, 124 (26), 7644–7645.
X.Q. Zhang, X. Xu, N. Bertrand, et al. Interactions of nanomaterials and biological systems: Implications to personalized nanomedicine. Advanced Drug Delivery Reviews. 2012, pp 1363–1384.
L. Yang, L. Zhang, T.J. Webster. Nanobiomaterials: State of the art and future trends. Advanced Engineering Materials. 2011.
A. Fedorov, R. Beichel, J. Kalpathy-Cramer, et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30 (9), 1323–1341.
K.D. Zschorsch. Catalytic combustion. In The John Zink Hamworthy Combustion Handbook, Second Edition: Volume 1 - Fundamentals; 2012; pp 137–157.
P.C. Lin, S. Lin, P.C. Wang, R. Sridhar. Techniques for physicochemical characterization of nanomaterials. Biotechnology Advances. 2014, pp 711–726.
T.W. Lin, L. Cardenas, L.J. Soslowsky. Biomechanics of tendon injury and repair. J. Biomech. 2004, 37 (6), 865–877.
N. Kumar, R. Kumar. Nanotechnology and Nanomaterials in the Treatment of Life-threatening Diseases; Elsevier, 2014.
W. Liu, Y. Li, J. Liu, et al. Application and Performance of 3D Printing in Nanobiomaterials. J. Nanomater. 2013, 2013, 1–7.
E.N. James, C. Hanna, L.S. Nair. Nanobiomaterials for Tissue Engineering Applications. In Stem Cell Biology and Tissue Engineering in Dental Sciences; 2015; pp 221–234.
E.S. Place, N.D. Evans, M.M. Stevens. Complexity in biomaterials for tissue engineering. Nat. Mater. 2009, 8 (6), 457–470.
F. Xu, F. Inci, O. Mullick, et al. Release of magnetic nanoparticles from cell-encapsulating biodegradable nanobiomaterials. ACS Nano 2012, 6 (8), 6640–6649.
V. Hasirci, E. Vrana, P. Zorlutuna, et al. Nanobiomaterials: A review of the existing science and technology, and new approaches. Journal of Biomaterials Science, Polymer Edition. 2006, pp 1241–1268.
F. Gelain. Novel opportunities and challenges offered by nanobiomaterials in tissue engineering. International Journal of Nanomedicine. 2008, pp 415–424.
L.G. Zhang, J.P. Fisher, K.W. Leong. 3D Bioprinting and Nanotechnology in Tissue Engineering and Regenerative Medicine; Elsevier, 2015.
H.S. Yoo, T.G. Kim, T.G. Park. Surface-functionalized electrospun nanofibers for tissue engineering and drug delivery. Advanced Drug Delivery Reviews. 2009, pp 1033–1042.
Refbacks
- There are currently no refbacks.
ISSN 2394-0867
 ISSN 2394-0867
ISSN 2394-0867